
Did you know that over 70% of patients believe their feedback leads to real changes in the care they receive? Yet, many healthcare organizations still struggle to harness this powerful resource. Patient feedback management is no longer optional—it's the essential driver for improving patient experience, increasing service quality, and transforming healthcare delivery.
This guide will teach you proven strategies to collect, analyze, and act on patient feedback, making measurable improvements in quality of care from day one.
Why Patient Feedback Management Is The Future Of Care Quality
Patients today are empowered with information and expect their voices to shape healthcare delivery. Patient feedback management is critical in helping healthcare providers strengthen quality of care, address operational issues, and foster a culture focused on patient-centered improvements. Healthcare organizations that listen to patient feedback are positioned to identify gaps in health service, adjust care processes, and tailor the patient journey for optimal satisfaction.
A thriving feedback system enables hospitals, clinics, and other care organizations to gather actionable insights and improve patient satisfaction. By analyzing feedback from patients, providers get a clear view of their strengths and weaknesses in real time—facilitating rapid cycles of service improvement. Robust patient feedback management also boosts trust by demonstrating that organizations value the patient voice and actively close the feedback loop for quality improvement.
Astonishing Truths: 70% of Patients Say Their Feedback Changes Care—Are You Listening?
Surveys reveal that a majority of patients believe that their feedback influences key decisions in healthcare organizations. However, only a minority feel that their concerns are addressed consistently. This gap highlights why effective patient feedback management systems must not only collect input, but demonstrate visible action and communication back to patients. For hospitals and clinics, closing this feedback loop is vital—it builds trust and reassures patients that their voices are truly valued, which directly boosts patient satisfaction and loyalty.
Proactively sharing feedback results and improvement initiatives with both staff and patients fosters transparency. Providers who champion patient experience data also showcase a commitment to continuous quality improvement. Ultimately, embracing robust patient feedback management not only elevates care organization reputation but helps improve patient care with every cycle of feedback and improvement.

Defining Patient Feedback Management: Scope, Significance, and Stakeholders
Patient feedback management is the structured process by which healthcare organizations collect, review, and apply feedback from patients across the health service continuum. Its scope spans inpatient admissions, outpatient services, specialty clinics, and even digital health platforms. At its core, the process is about transforming direct patient stories, ratings, and suggestions into actionable steps for service improvement.
Key stakeholders in patient feedback management include not only patients and their families, but also front-line clinicians, hospital administrators, quality analysts, and IT teams responsible for feedback system technology and integrations. The overarching significance of this process is the direct connection between feedback data and real, measurable increases in service quality and patient satisfaction. Each stakeholder plays a vital role in gathering, interpreting, and acting on feedback to enhance the healthcare experience at every touchpoint.
Developing a Culture of Transparency with Patient Feedback Systems
Building a culture of transparency means weaving patient feedback into the organization’s daily operations and decision-making processes. A transparent approach to feedback means making results visible and accessible—not just to leaders and regulators, but to all staff and the patients themselves. This openness encourages honest participation, reduces fear of reprisal or judgment, and motivates teams to seek ongoing improvement.
Clinicians and administrative staff are more likely to engage constructively with improvement initiatives when they see the direct impact of feedback on patient care. Regularly sharing progress updates, celebrating achievements, and acknowledging areas needing growth are best practices for reinforcing a positive culture. When healthcare providers champion transparency, patients feel respected and heard, which translates into higher engagement and satisfaction rates.

Understanding Patient Feedback Management In Healthcare
Patient feedback management is an evolving discipline in healthcare, aimed at continuously improving patient experience and service quality. Understanding the different types of patient feedback and leveraging advanced feedback management systems enables organizations to act quickly and decisively. Healthcare providers who fine-tune their strategies around patient satisfaction and feedback data gain valuable insights, transforming feedback into actionable, organization-wide improvement.
Collecting feedback from patients at various stages of the patient journey is essential for uncovering patterns and trends. Whether feedback is structured via surveys or unstructured via open comments, effective systems ensure nothing is lost in translation. By viewing patient feedback management through both strategic and tactical lenses, organizations can consistently deliver higher standards of patient care and satisfaction.
Types of Patient Feedback: Structured Versus Unstructured
There are two main types of patient feedback: structured and unstructured. Structured feedback typically comprises standardized satisfaction surveys, rating scales like the 5-point Likert scale, and quantifiable questionnaires. These formats produce data that is easily aggregated, analyzed, and benchmarked—ideal for tracking patient experience trends over time and measuring specific aspects of health care quality.
Unstructured feedback, on the other hand, includes open-ended survey responses, individual comments, and direct narratives shared during care or online. While harder to quantify, unstructured feedback offers rich, contextual insights into the complexities of the patient journey. A robust feedback management system captures both types, providing a holistic view of the patient experience and equipping healthcare providers to address concerns from all angles.
The Feedback System: From Collection To Analysis In Health Care
The feedback system forms the backbone of patient feedback management, encompassing every stage from data collection to in-depth analysis. Modern systems gather feedback via multiple touchpoints—post-discharge surveys, real-time kiosks, mobile apps, and digital platforms. This multi-channel approach ensures that feedback from patients is both abundant and inclusive of diverse perspectives.
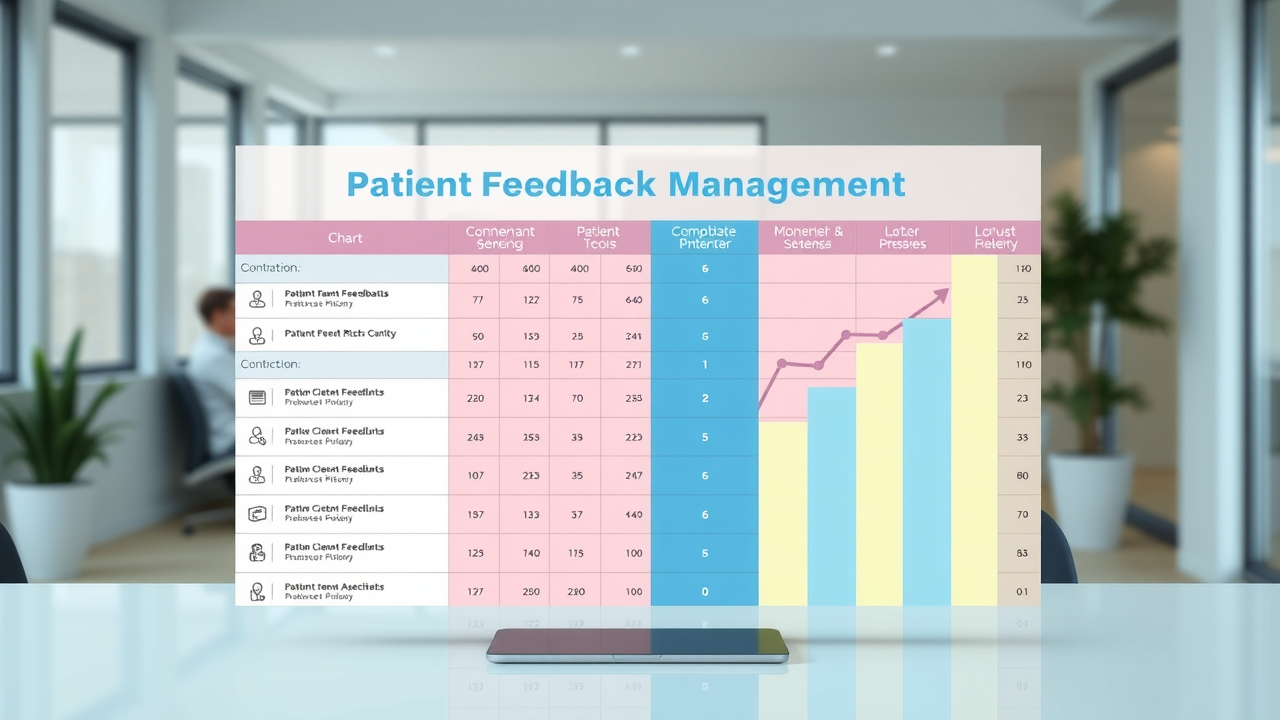
Once collected, feedback data must be swiftly sorted, categorized, and analyzed for actionable trends. Automated data analysis tools can rapidly identify recurring issues, satisfaction gaps, and highlight potential service improvement opportunities. By integrating feedback system data with other patient care metrics, organizations gain a comprehensive understanding of their strengths and areas needing improvement—enabling a precise, data-driven approach to quality improvement initiatives.
Leveraging Feedback Data: Transforming Insights Into Service Improvement
The true value of patient feedback management lies in the transformation of raw feedback data into targeted quality improvement initiatives. Healthcare organizations should regularly review and interpret satisfaction surveys and unstructured comments, using them to fuel both service improvement planning and real-time operational adjustments. This continual cycle fosters a learning organization where every stakeholder is empowered to drive patient-centered innovation.
Data-driven healthcare providers can benchmark performance, monitor patient satisfaction trends, and prioritize improvements that will have the greatest impact on patient experience. Implementing dedicated feedback loops—where action taken in response to patient feedback is documented and communicated—helps to build a culture of accountability and transparency. Over time, this approach leads to measurable gains in patient care, stronger trust, and improved organizational reputation.

Driving Service Quality With Actionable Patient Feedback
Actionable patient feedback is the cornerstone of advanced service quality strategies in modern healthcare. By capturing real-time experiences and sentiment, providers can make swift, targeted interventions that directly improve the quality of care. Whether addressing operational bottlenecks or refining bedside manner, patient feedback management directly shapes an organization’s service reputation and ongoing success.
Service quality flourishes in organizations that move quickly from data collection to decisive action. Integrating patient satisfaction surveys and feedback analytics into regular quality improvement meetings transforms theory into practice, ensuring every suggestion or criticism is a step towards better health care outcomes.
Enhancing Patient Experience Through Real-Time Feedback Systems
Real-time feedback systems offer patients multiple ways to share experiences as they happen—through bedside tablets, SMS surveys, or touchpoints embedded in patient portals. This immediacy gives healthcare providers important, up-to-the-minute insights that can resolve small concerns before they become major complaints. Moreover, these dynamic systems empower patients to influence services throughout their patient journey, not just at the end of care episodes.
Clinicians and health service managers can monitor feedback dashboards to spot trends quickly, such as delays, communication breakdowns, or facility issues, and intervene on the same day. The responsiveness enabled by real-time feedback is a game-changer, positioning patient feedback management as both a diagnostic and a continuous improvement tool for optimizing patient care.
Improvement Initiatives Based On Patient Satisfaction Surveys
Patient satisfaction surveys provide structured, numerical insight into many areas of health care, such as wait times, staff courtesy, cleanliness, and information clarity. When organizations systematically analyze this data, they can prioritize improvement initiatives that matter most to their patients. For example, consistently low scores in communication can drive new training for staff or changes to care protocols.
The most successful healthcare providers use satisfaction survey results to initiate both big-picture change and small, rapid quality improvements. By linking survey themes to measurable goals, organizations align improvement initiatives with patient-centered priorities, strengthening both trust and outcomes. A transparent approach, sharing survey findings and planned changes with all stakeholders, further amplifies the positive impact on patient satisfaction and health service quality.

Best Practices for Feedback Management Across Healthcare Providers
Consistent, organization-wide best practices make patient feedback management truly effective across healthcare providers. Key practices include leveraging multi-channel feedback collection, standardizing data analysis, and fostering open dialogues between patients and healthcare teams. Hospitals that conduct routine feedback reviews, share results transparently, and implement staff recognition programs for patient-positive changes consistently rank higher in service quality and patient satisfaction.
It’s also important that every healthcare provider integrates feedback management into their daily workflows with dedicated feedback champions. Effective feedback systems should allow staff to quickly escalate concerns, track resolution progress, and close the feedback loop with patients. These best practices make continuous improvement possible, raising the bar for healthcare experience across facilities and specialties.
Leveraging Technology For Patient Feedback Management
Digital platforms, AI-powered sentiment analysis, and user-friendly dashboards are transforming how care organizations manage feedback from patients. Automated tools enable providers to sift through thousands of survey results and comments, flagging urgent issues and surfacing common themes that drive service improvement.
Mobile apps and web-based portals increase accessibility, encouraging higher response rates and more diverse feedback. Advanced technology also supports integration with electronic health records and other core healthcare systems, streamlining data use for direct care improvement. The result is a feedback loop that is faster, more actionable, and able to deliver significant advances in quality of care.

Implementing A Robust Patient Feedback System In Your Organization
To reap the full benefits of patient feedback management, healthcare organizations must build robust systems tailored to their unique needs. This process starts with selecting a suitable feedback system, training staff, and ensuring seamless workflow integration. A strong feedback management system supports the entire journey from data collection to clear, actionable service improvement, making it a strategic asset for any care organization aiming to improve patient experience and satisfaction.
Successful implementation involves all levels of staff, from nurses to senior executives, and includes regular evaluation and adaptation of feedback strategies. Regularly monitoring feedback results, conducting root cause analysis, and benchmarking against industry standards help advance the organization on its patient-centered improvement journey.
Choosing The Right Feedback System: Features To Look For
When selecting a feedback management system, key features should include user-friendly survey creation, automatic data aggregation, smart analytics and reporting tools, and secure integration with other hospital systems. Look for platforms that offer multi-language support, real-time data visualization, and the ability to customize feedback channels for diverse patient populations. HIPAA compliance and robust data security must also be top priorities for patient trust and regulatory assurance.
Systems with automated alerting and workflow modules help teams quickly respond to urgent feedback, track improvement initiatives, and close the feedback loop. These capabilities ensure that the patient experience is at the forefront of service quality efforts, driving real results across the care organization.
Training Staff To Improve Patient Experience With Feedback Data
Staff training is critical to translating patient feedback management into tangible improvements for patient care. Training should focus on interpreting feedback data, identifying actionable trends, and developing empathetic communication skills. Regular workshops and e-learning modules can empower all team members—from frontline staff to leadership—with the confidence and tools to act on feedback swiftly and effectively.
Embedding feedback-focused objectives into staff performance reviews and recognition systems further ensures that service improvement becomes an ongoing priority. When staff feel supported and see the impact of their efforts reflected in patient experience and satisfaction scores, engagement and morale rise—fuelling a powerful, positive feedback loop throughout the organization.
Workflow Integration: Closing The Loop On Patient Feedback
Integrating patient feedback management into daily workflows unlocks the power of continuous quality improvement. This requires clear procedures for collecting and escalating feedback, systems for tracking follow-up actions, and regular reporting on progress. Automated tools can support workflow integration by routing alerts to relevant staff and providing timely updates to both patients and care teams.
Closing the feedback loop—informing patients about changes made as a result of their feedback—reinforces trust and encourages future participation. Effective integration means that feedback is not a standalone process, but an embedded element of care delivery, contributing to lasting improvements in both patient satisfaction and quality of care.
Designing Effective Patient Satisfaction Surveys
The foundation of patient feedback management is a well-designed satisfaction survey that captures authentic patient experiences. Crafting surveys that are concise, clear, and relevant ensures reliable data collection and high response rates. An effective survey design leverages the right measurement tools—like the 5-Point Likert Scale—and asks targeted questions to elicit meaningful, actionable feedback.
Surveys should be trialed and validated with real patients before wide distribution. This quality assurance step ensures clarity and maximizes the actionable value of survey data. Ultimately, the right questions coupled with the right format lead to better insights, empowering care organizations to implement impactful improvement initiatives.
The 5-Point Likert Scale For Patient Satisfaction: How To Use It Well
The 5-Point Likert Scale is the gold standard for measuring patient satisfaction across a spectrum from “Very Dissatisfied” to “Very Satisfied.” It transforms subjective experiences into quantifiable data, making it possible to compare results across clinics, track year-over-year changes, and pinpoint areas needing attention. When used skillfully in surveys, the Likert Scale provides both high-level benchmarking and granular detail, supporting targeted quality improvement.
For best results, integrate the Likert Scale alongside open-ended questions, providing a balance between measurable insights and rich, qualitative feedback. Healthcare providers should regularly analyze Likert Scale results by department, clinician, or service line—rapidly identifying excellence and areas for improvement in their patient journey.
Question Formulation: Ensuring Quality Insights From Your Patient Feedback
Strong survey design depends on the quality of questions asked. Effective patient feedback management focuses on drafting questions that are specific, unbiased, and aligned with patient priorities. Instead of vague or generic queries, use targeted phrasing: “How satisfied were you with staff explanations of your treatment?” or “Did you feel respected during your visit?”--questions that speak directly to the care experience.
Pilot testing questions with a small patient sample helps to clarify ambiguous wording and ensures the survey is not overly long or complex. When surveys are consistently reviewed and refined, organizations gather higher quality feedback data, making it easier to drive successful improvement initiatives based on patient experience.

Boosting Response Rates: Strategies To Maximize Feedback From Patients
Maximizing feedback survey response rates ensures data reflects the full diversity of patient experiences. Strategies include making surveys easily accessible via email, SMS, app, or in-person kiosks, providing language and accessibility options, and keeping surveys short but targeted. Clear invitations expressing the impact of patient feedback—such as messages explaining how data is used to improve patient care—encourage participation.
Sending reminders, ensuring surveys are anonymous, and offering small incentives can also improve response rates. The more patients who participate, the richer and more accurate the experience data, supporting comprehensive improvement initiatives and boosting service quality across every stage of the patient journey.
Interpreting And Acting On Patient Feedback Data
The strength of patient feedback management is realized when organizations systematically interpret feedback data and launch measurable service improvements. Robust data analysis processes—such as trend monitoring, root cause analysis, and predictive modeling—transform raw responses into actionable intelligence. Acting promptly on analysis ensures that feedback is not just collected, but actively used to enhance patient experience at every level.
Continuous data interpretation enables healthcare organizations to set clear targets, adjust strategies, and communicate outcomes back to patients and staff. When feedback analysis is routine, it fosters a responsive, high-performing care organization attuned to evolving patient needs.
Data Analysis—Turning Patient Feedback Into Measurable Healthcare Experience Gains
Comprehensive data analysis translates thousands of survey responses and patient comments into key trends and quantifiable metrics. Whether using manual review or advanced analytics software, providers can quickly identify opportunity areas—such as communication gaps, safety concerns, or facility issues—impacting the healthcare experience. The value of feedback data shines when insights are turned into clear action plans, measurable outcomes, and evidence-based improvement initiatives.
Healthcare organizations should track metrics such as Net Promoter Scores (NPS), satisfaction by department, and trend shifts after implementing changes. This process supports continuous quality improvement and demonstrates the tangible impact of patient feedback management on service quality and patient outcomes.
Monitoring Trends In Patient Satisfaction And Service Quality
Monitoring trends is vital for spotting long-term shifts in patient experience and addressing emerging challenges. Regular trend analysis of feedback system data highlights consistent service improvement wins, as well as areas at risk for declining satisfaction. Organizations should evaluate trends by demographics, visit types, and procedures to identify differential impacts and equity concerns.
Sharing trend reports with clinicians, quality teams, and leadership creates a shared understanding and promotes coordinated, rapid response. Integrated, real-time dashboards give all stakeholders access to up-to-date indicators of patient satisfaction and healthcare service quality, strengthening data-driven decision-making across the organization.
Reporting Feedback Outcomes To Stakeholders
Transparent, timely reporting of feedback outcomes solidifies trust and closes the feedback loop with both patients and internal teams. Leadership should regularly communicate findings, improvement initiatives, and measurable results from patient feedback management efforts through newsletters, staff meetings, and patient forums. This open reporting builds a sense of ownership and accountability at all levels of the care organization.
Cultivating feedback-informed communication ensures that every stakeholder understands both the value of feedback data and the ongoing efforts to improve patient experience and healthcare service quality. Sustained transparency enhances the organization’s reputation for being responsive to the needs and voices of its patients.

Handling Negative Feedback: Turning Criticism Into Improvement Initiatives
Negative feedback is a catalyst for service improvement, not a cause for defensiveness. Healthcare organizations should view criticism as an opportunity to identify blind spots and proactively address underperforming areas of the patient journey. Immediate acknowledgment, careful analysis, and clear communication of improvement actions are best practices for managing negative feedback successfully.
By closing the loop and reporting specific changes—such as new training, updated protocols, or service enhancements—care organizations show a genuine commitment to patient-centered excellence. This approach transforms even the harshest criticism into powerful drivers for quality improvement and strengthens patient loyalty over time.
Overcoming Challenges In Patient Feedback Management
While patient feedback management holds great promise, it also presents challenges—especially in areas like privacy, staff engagement, and patient participation. Addressing these roadblocks head-on is essential for building a resilient and effective feedback system that drives continuous improvement and enhanced care outcomes.
Strategies for overcoming these challenges range from adopting advanced data security measures to combating burnout and fostering a safe, open environment for honest patient feedback. When organizations proactively tackle barriers, they unlock the full potential of feedback for service quality enhancement.

Privacy, Security, And Trust In The Feedback System
Privacy and data security concerns can limit willingness to share honest feedback—unless organizations go above and beyond to safeguard patient information. Ensuring surveys are anonymous, adopting encrypted digital feedback platforms, and clearly communicating privacy policies are vital to building trust in the feedback system.
Compliance with regulations such as HIPAA and transparent data handling protocols further secure patient confidence. By prioritizing privacy and security, healthcare organizations not only protect sensitive experience data but also encourage more open and thorough feedback, benefiting all aspects of care quality and improvement initiatives.
Combating Feedback Fatigue Among Healthcare Providers And Patients
Feedback fatigue can affect both staff and patients when surveys are too frequent, repetitive, or lengthy. Careful scheduling of surveys—timing them thoughtfully and ensuring relevance—keeps participation high while preventing burnout. Rotating the focus of questions and periodically refreshing survey formats also keeps feedback systems engaging and effective.
Empowering staff to suggest improvements to feedback processes and involving patients in survey design are proven strategies to sustain engagement. By valuing the time and opinions of all participants, care organizations build a more resilient and energizing feedback culture, boosting both service quality and satisfaction outcomes.
Encouraging Honest Patient Participation For Better Feedback Data
Honest, candid feedback lies at the heart of meaningful service improvement. Organizations can foster trust by conveying the value of participant opinions, assuring anonymity, and acting visibly on collected feedback. When patients see real changes resulting from their input—such as new policies or service upgrades—they are more likely to share detailed, honest experiences in the future.
Healthcare organizations should also provide safe, multiple channels for feedback (online, phone, in-person) to accommodate diverse preferences and comfort levels. Celebrating internal case studies of service improvement initiatives powered by patient feedback further motivates honest participation.

Future Trends In Patient Feedback Management And Service Quality
The future of patient feedback management is being shaped by advanced technology, increased personalization, and strategic alignment with broader healthcare quality goals. Embracing these trends enables healthcare providers to stay ahead in delivering exceptional patient experiences while maximizing value and efficiency across all health services.
Stakeholders at every level should be aware of and adapt to these evolving trends to maintain best-in-class feedback management strategies and sustain long-term health care transformation.
The Rise Of AI And Automation In Feedback Systems
Artificial intelligence and automation are revolutionizing patient feedback management. These tools rapidly process large volumes of feedback data, identifying sentiments, urgent complaints, and improvement opportunities with remarkable efficiency. Automated alerts and dashboards allow staff to address problems in real time and implement quality improvement initiatives faster than ever before.
AI-driven analytics can also uncover hidden patterns and suggest predictive interventions, helping organizations stay ahead of trends in patient satisfaction and service quality. By harnessing AI, care organizations make feedback management agile, responsive, and scalable.

Personalization: Tailoring Care Based On Patient Feedback Insights
Personalization is the next frontier in patient feedback management. Integrating feedback insights with electronic medical records enables providers to customize care plans, communication, and follow-up based on individual experiences and preferences. This approach not only strengthens patient engagement but also improves clinical outcomes and overall satisfaction.
Personalized interventions—such as targeted education, custom discharge instructions, or bespoke appointment reminders—can directly address recurring issues raised in feedback data. Personalization turns generalized service improvement into highly relevant, individual care enhancements that truly resonate with patients.
Aligning Feedback Management With Broader Healthcare Quality Goals
Top-performing care organizations are aligning feedback management strategies with their larger quality improvement frameworks. Doing so ensures that patient experience data is not just collected, but leveraged to drive organization-wide transformation in safety, clinical effectiveness, and equitable access. In this way, patient feedback management becomes an integral part of achieving—and demonstrating—sustained excellence in healthcare services.
When executive leadership, quality departments, and clinical operations are united in harnessing feedback insights, the organization’s ability to respond rapidly and effectively is greatly enhanced. Continuous alignment ensures that improvement initiatives powered by patient feedback translate into lasting gains across all aspects of health care delivery.

Harness the Power of Patient Reviews to Elevate Your Practice
Patient reviews have become a cornerstone of modern healthcare, shaping how practices are perceived and chosen by patients. Beyond building credibility, they serve as a valuable source of feedback that can guide improvements in care, communication, and overall patient experience. Practices that consistently engage with reviews are better equipped to identify strengths, address concerns, and demonstrate accountability.
A strong patient reviews strategy also provides a competitive edge in an increasingly digital landscape. Positive feedback enhances online visibility, supports patient trust, and helps practices stand out in crowded markets. When effectively managed, reviews can drive long-term success by strengthening reputation, fostering loyalty, and creating a cycle of continuous growth and improvement.

Frequently Asked Questions About Patient Feedback Management
Why is patient feedback important for medical practices?
Patient feedback is essential because it gives healthcare providers a direct view of the patient experience. It helps identify what is working well, such as quality of care and communication, while also pointing out areas that need improvement. When acted on, feedback leads to better patient satisfaction, improved outcomes, and stronger trust between patients and providers.
How can healthcare providers collect patient feedback effectively?
The most effective way is to offer multiple channels for patients to share their thoughts. This can include digital surveys sent after appointments, online review platforms, patient portals, or even short text message polls. In-office methods like comment cards or tablets in waiting rooms can also work. The key is to make feedback easy, convenient, and accessible for patients of all ages and comfort levels.
What’s the best way to handle negative reviews or feedback?
The best approach is to respond promptly, professionally, and with empathy. Acknowledge the patient’s concerns without being defensive, and if possible, outline steps your practice will take to address the issue. This shows that you value feedback and are committed to making improvements. Often, a thoughtful response can turn a negative experience into a chance to build trust and even retain the patient.
Can patient feedback improve online reputation?
Absolutely. Positive patient reviews help boost your visibility on search engines and review platforms, which makes your practice more appealing to potential patients. When prospective patients see that others had positive experiences, it builds credibility and trust. Even handling negative reviews the right way can enhance your reputation by showing you are responsive and patient-focused.
How often should practices review and analyze patient feedback?
Practices should monitor feedback consistently—ideally every week or at least monthly. Regular review ensures issues are addressed quickly and allows patterns to be identified, such as recurring concerns about wait times or communication. Over time, this continuous monitoring supports a culture of improvement and ensures patients feel heard and valued.

Take the Next Step: Transform Patient Feedback Into Lasting Care Excellence
Patient feedback is more than just reviews—it’s a roadmap to building trust, improving outcomes, and strengthening your practice’s reputation. By actively listening to patients and integrating their insights into daily operations, you can uncover opportunities to enhance communication, streamline processes, and deliver care that truly meets patient needs. Don’t wait to elevate your practice—start implementing a patient feedback management strategy today and create a lasting culture of excellence that sets your healthcare practice apart.
 Add Row
Add Row  Add
Add 




Write A Comment